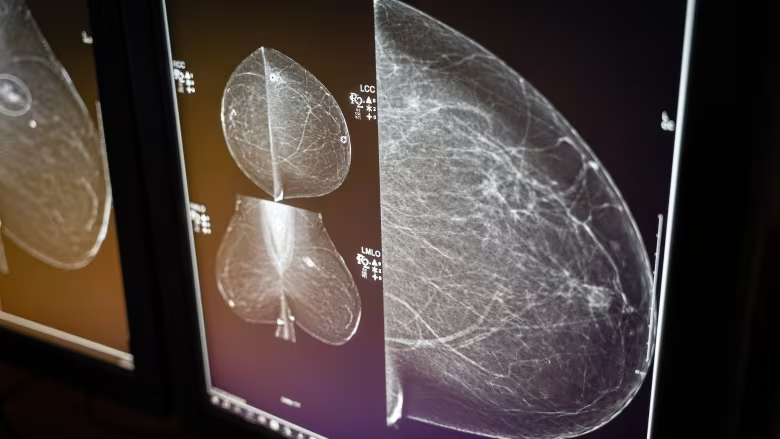
A group of experts say the Canadian Task Force on Preventive Health Care's recommendations are outdated and lagging behind what other jurisdictions are doing to detect various forms of cancer early. (CBC News)
Carolyn Holland reflects on her battle with breast cancer, pondering the years she might have saved had her diagnosis come sooner. She discovered lumps at 43, prompting aggressive treatment. Her experience underscores concerns over Canada's outdated cancer screening guidelines, criticized for overlooking high-risk individuals like her.
Holland's journey began with a self-discovery of breast lumps during a routine shower, a pivotal moment that led to a cascade of medical interventions. At 43, she had never undergone a mammogram, a decision she now questions given the trajectory of her illness.
Upon consulting her doctor, Holland underwent a scan that confirmed her fears: cancer had taken root, already advanced by the time of detection. The ensuing treatment regimen was grueling, encompassing chemotherapy, radiation, lymph node removal, and a double mastectomy.
Holland's frustration is palpable as she contemplates the preventable nature of her ordeal. She believes timely screening could have spared her from the harsh realities of her treatment journey. Her doctors concur, suggesting that earlier detection might have led to less invasive measures.
Yet, the crux of Holland's plight lies in Canada's national guidelines, which fail to advocate routine breast cancer screening for women under 50. Had she been afforded access to mammograms at 40, she asserts, her outcome might have been vastly different.
The issue transcends Holland's personal narrative, echoing in the voices of medical experts who decry the entrenched reliance on outdated screening protocols. Led by the Canadian Task Force on Preventive Health Care, these guidelines shape clinical practice nationwide.
Dr. Shiela Appavoo, a prominent Edmonton-based radiologist, spearheads the Coalition for Responsible Healthcare Guidelines. The coalition comprises cancer specialists, family doctors, and concerned patients advocating for guideline reforms.
Their contention is that the task force's recommendations are rooted in antiquated research, lacking the agility to incorporate evolving scientific insights. Moreover, the task force's reluctance to promptly update its directives exacerbates the risk of delayed diagnoses and compromised outcomes.
The impending update to breast cancer screening guidelines offers a glimmer of hope, slated for next month. However, the current stance, last revised in 2018, discourages broad screening for women in their 40s, a policy shift that the Canadian Cancer Society has contested.
Several provinces have bucked the national directives, extending screening eligibility to younger cohorts. British Columbia, Nova Scotia, P.E.I., and Yukon have proactively lowered the screening age threshold, acknowledging the imperative of early detection.
Yet, Appavoo underscores a pervasive adherence to national guidelines among family physicians, despite localized variations in screening practices. This disconnect perpetuates disparities in access to critical screening measures, hindering efforts to combat cancer effectively.
The situation extends beyond breast cancer, encapsulating other malignancies like cervical, lung, and prostate cancer. In each domain, task force guidelines lag behind global benchmarks, impeding timely diagnoses and optimal patient care.
Dr. Anna Wilkinson, an Ottawa-based family physician, bemoans the repercussions of rigid adherence to outdated guidelines. She recounts instances where patients in their 40s, seeking mammograms, were rebuffed due to guideline constraints, a scenario she deems "heartbreaking."
Wilkinson's advocacy for evidence-based reforms mirrors a broader call for action within the medical community. The onus lies on the task force to heed the clarion call for guideline modernization, aligning clinical practice with contemporary standards.
Amidst these challenges, the enduring plight of cancer patients underscores the urgency of reform. As Holland aptly observes, the task force's inaction not only undermines patient well-being but also perpetuates avoidable suffering.















