Photo from Onclive.com
Health Canada recently granted approval for the use of a subcutaneous form of atezolizumab, known as Tecentriq, in treating patients with lung cancer, breast cancer, or hepatocellular carcinoma (HCC). This approval applies to cases where the intravenous (IV) form of the drug has already been approved.
The decision to approve the subcutaneous formulation was supported by data from part 2 of the phase 1b/3 IMscin001 trial (ClinicalTrials.gov identifier: NCT03735121). This trial demonstrated that administering atezolizumab subcutaneously resulted in comparable levels of the drug in the bloodstream compared to the IV formulation. The trial successfully met its primary objectives related to the concentration of the drug in the blood during the first treatment cycle and over a 21-day period.
Specifically, the study found that the concentration of atezolizumab in the blood during the first treatment cycle was similar between the subcutaneous and IV formulations. Additionally, the overall exposure to the drug over the 21-day period was slightly lower with the subcutaneous formulation compared to the IV formulation.
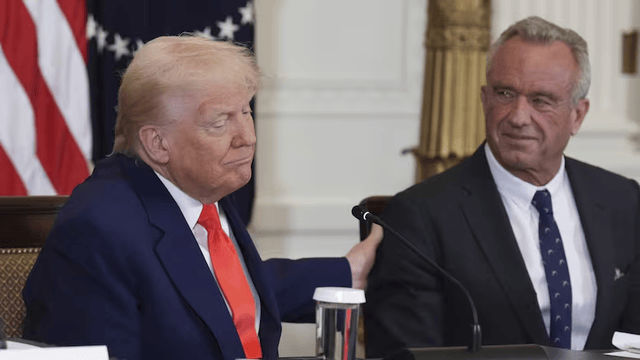
Dr. Sara Moore, a medical oncologist at The Ottawa Hospital, emphasized the potential benefits of subcutaneous administration, particularly in reducing the burden of treatment for patients. She highlighted the challenges patients face, including managing family, social, and financial responsibilities, as well as the logistical difficulties associated with frequent visits to infusion centers. Dr. Moore emphasized that subcutaneous treatment options could alleviate some of these burdens, especially for patients in rural or remote areas who may face challenges accessing infusion centers.
In January 2024, the European Commission also approved subcutaneous atezolizumab co-formulated with Enhanze, a recombinant human hyaluronidase enzyme, for all indications previously approved for the IV formulation. This decision was based on similar data from the IMscin001 trial.
The IMscin001 trial enrolled patients with locally advanced or metastatic non–small cell lung cancer who had received prior treatment with platinum-containing regimens or experienced disease recurrence after prior platinum-based neoadjuvant or adjuvant therapy. Patients were required to meet specific criteria related to their overall health and disease status.
Patients enrolled in the trial were randomly assigned to receive either subcutaneous or IV atezolizumab once every three weeks. The study assessed various endpoints, including steady-state exposure, efficacy, safety, and immunogenicity.
Results from the trial showed that progression-free survival, objective response rate, and incidence of anti-atezolizumab antibodies were similar between patients receiving the subcutaneous and IV formulations. Importantly, no new safety concerns were identified.
Michelle Forman, an oncology nurse at Burnaby Hospital Cancer Centre, highlighted the practical benefits of subcutaneous immunotherapy for patients and healthcare providers. She emphasized reduced clinic time, less invasive administration, and greater flexibility in scheduling treatment. Additionally, she noted that subcutaneous administration allows for treatment closer to home, which can reduce the stress associated with travel for patients.
In summary, the approval of subcutaneous atezolizumab by Health Canada represents a significant advancement in cancer treatment, offering patients a potentially more convenient and accessible option for therapy.